Modified cells survived 19 months after transplant into an HIV-positive man in China, but the dose was not enough to reduce his viral load.
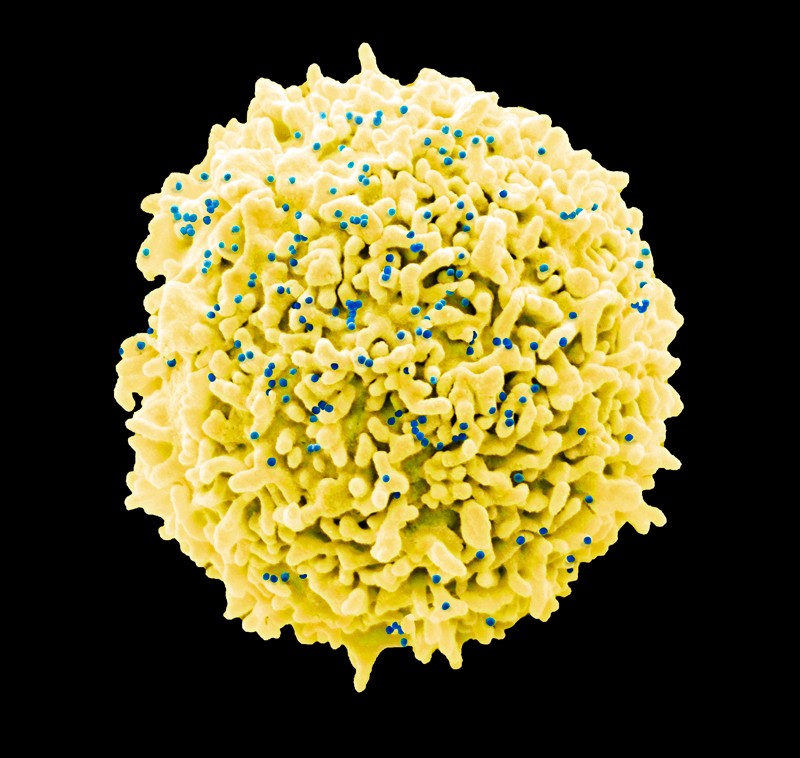
HIV destroys the body’s defences by attacking immune cells. Credit: Steve Gschmeissner/Science Photo Library
For the first time, researchers have used CRISPR gene-editing technology to try to treat a person infected with HIV.
Scientists in China engineered human stem cells to mimic a rare form of natural immunity to the virus and transplanted them into a man with HIV and blood cancer. The gene-edited cells survived in the man’s body for more than a year without causing detectable side effects, but the number of cells was not high enough to significantly reduce the amount of HIV in his blood.
“This is an important step towards using gene editing to treat human disease,” says Fyodor Urnov, a biologist at the University of California, Berkeley. “Because of this study, we now know that these edited cells can survive in a patient, and they will stay there.”
The study1 was published on 11 September in The New England Journal of Medicine. Lead author Hongkui Deng, a biologist at Peking University in Beijing, says that the research was inspired by a remarkable bone-marrow transplant that seemingly cured a man of HIV more than a decade ago.
Mutant power
In 2007, Timothy Ray Brown ― initially known as ‘the Berlin patient’ ― underwent a bone-marrow transplant to treat his leukaemia. The bone-marrow donor was special, however, in that he had a version of the CCR5 gene that confers immunity to HIV.
Normally, the gene encodes a receptor on the surface of white blood cells that the HIV virus uses to infiltrate cells. But in people with two copies of the CCR5 mutation, this receptor is warped and blocks certain strains of HIV from entering cells. The HIV-resistant version of the gene is exceptionally rare: it’s found in just 1% of people of European descent, and is virtually nonexistent in other ethnic groups.
Doctors hoped that the bone-marrow transplant would replace Brown’s HIV-susceptible blood cells with immune ones — and it did. After nearly 13 years, there is no sign of HIV in his blood, and his leukaemia is in remission. In March, researchers reported that a second person underwent a similar procedure in Britain and was cured2.
Deng wanted to use CRISPR gene editing to engineer HIV-resistant blood stem cells from normal donors, making this potential cure more widely accessible. He and his colleagues tested this approach on a 27-year-old man in China who had been diagnosed with HIV and leukaemia, and who needed a bone-marrow transplant. The scientists extracted bone-marrow stem cells from a donor and used CRISPR–Cas9 to transform them into CCR5 mutants.
At first, the researchers couldn’t get CRISPR to knock out CCR5 in the stem cells. “I thought, wow, these cells are really tough,” says Deng. Eventually, the were able to edit 17.8% of the donor’s stem cells.
Safety first
To maximize the chance that the transplant would treat the patient’s cancer, the researchers mixed the edited stem cells with unedited ones. The team monitored the man after the transplant to see whether the edited cells would survive and replicate, whether they treated the HIV infection and, most importantly, whether the treatment was safe.
“This was the first trial, so the most important thing was to test safety,” says Deng.
CRISPR gene editing in people remains controversial, in part because many researchers worry about its side effects. Studies have shown that CRISPR sometimes creates unwanted mutations in the lab3 — and the consequences of that happening in a person could be disastrous.
After 19 months, the CRISPR-edited stem cells did persist, although they comprised only 5–8% of the recipient’s total stem cells. This means that a little over one-half of the edited cells died after they were transplanted. And although the man’s leukaemia is in remission, he is still infected with HIV.
“I’m not surprised that 5% was not enough to lower the viral load,” says Urnov, “but now we know that CRISPR-edited cells can persist, and that we need to do better than 5%.”
To Deng, the most important thing is that the man did not suffer any side effects caused by the gene-edited cells. And when the researchers sequenced the genomes of those cells, they didn’t find evidence of unintended genetic changes.
Pushing forward
“This is really good news for the field,” says Carl June, an immunologist at the University of Pennsylvania in Philadelphia. “We now know that, in principle, we can use CRISPR to edit human stem cells, that they can persist in a patient and that it can be safe.”
June says that this proof of concept opens the door for research into testing this technology for treatment of other blood diseases, such as sickle-cell anaemia. He also notes that this study complied with standard ethical protocols, including obtaining informed consent from the participant.
Improvements in gene-editing technology mean researchers can now edit stem cells with efficiency greater than the 17.8% success rate in the latest study. But that comes with risks. Each time CRISPR makes cuts in the genome, there’s a chance something could go wrong. Editing cells more efficiently means making more cuts, and creates more opportunity for mistakes.
“This paper is an incomplete success, but it will only motivate the field to push onwards,” says Urnov. Had the experiment proved to be unsafe, regulatory agencies might have stopped future research. Now, he says, researchers can point to this study as proof of concept that this line of research can be safe and potentially fruitful.
“I’m going to have an extra scoop of ice cream tonight, knowing that the ship of human genome editing for treating disease is still on course,” says Urnov.
(원문: 여기를 클릭하세요~)